News Spotlight: Humanity in Corrections - Suicide Prevention in Prisons
July 14, 2023
- About
- Suicide Prevention Plans
- Recommendations from Lindsay Hayes
- Challenges Unique to Prisons
- Common Myths about Suicide
- DOC’s Commitments to Suicide Prevention Moving Forward
- Resources
About
According to the Centers for Disease Control and Prevention, suicide is one of the leading causes of death in the United States. As state prisons mirror the population, this means that individuals incarcerated in prison are not exempt from the risk of suicide and often can be at an increased risk. The National Institute of Corrections warns us that the rates of suicide in those who are incarcerated are often much higher than those of the population because taking away a person's liberty has a deep impact on their overall wellbeing.
The Washington State Department of Corrections (DOC) recently experienced an increase in the number of suicides and suicide attempts. Five incidents, four suicides and one attempted suicide, occurred over a 35-day period at two of our major facilities, Washington State Penitentiary BAR Units (Baker, Adams, Rainier) and Monroe Correctional Center Sky River Treatment Center (SRTC). Four of those five attempts occurred within a five-day period between June 10th – June 15th.
This many incidents in such a short period of time is rare and warrants a close review. DOC is thoroughly reviewing and evaluating each occurrence. While these root cause evaluations take time to complete and will be reported on in the Unexpected Fatality Report, DOC feels it is in the public’s interest to provide information on suicide prevention in state run prisons to help bring awareness to this important topic.
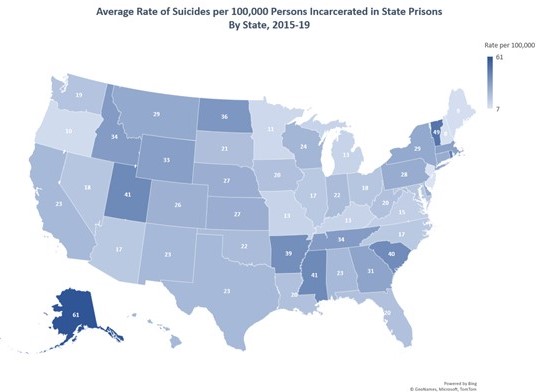
Map of National Rate of Suicides per 100,000 Persons Incarcerated in State Prisons from 2015-2019
Suicide Prevention Plans
DOC has comprehensive suicide prevention plans in place at all DOC facilities. Unfortunately, as in the broader community, not all suicide attempts can be prevented. However, these prevention plans are an important step in ensuring the mental health of those in our care and custody.
Situational awareness remains one of the most important prevention strategies. This is achieved by having well-trained staff present and checking in with incarcerated individuals regularly.
Staff are encouraged to have regular communication with individuals. We want people to know that they can tell us when they are struggling. We want them to know that we want to help. In addition to staff presence, one of the methods to raise awareness within the population are posters that have been developed (pdf) and distributed to Health Services clinics within prisons to post in visible areas. These posters are also available for use in all living units and other areas:
Another important part of prevention is the agency Critical Incident Review and the legislatively required Unexpected Fatality Review processes. By investigating each individual occurrence and conducting a Psychological Autopsy, this allows us to better understand the circumstances and allow for analyses of possible common patterns or triggering factors and any circumstances leading up to a suicide that can be used for prevention methods in the future.
Recommendations from Lindsay Hayes
The department invited national suicide expert Lindsay Hayes to visit our prisons and make recommendations to improve suicide prevention practices.
Some of these recommendations and DOC’s status on implementation are as follows:
| Recommendation | DOC Status |
|---|---|
| Development of an alert screen in OMNI to indicate previous history of suicidal behavior while in DOC. | Completed |
| Determine costs associated with private, confidential settings for mental health screenings at reception and restrictive housing units. | All restrictive housing units have established private confidential settings for mental health screenings/evaluations. Washington Corrections Center (WCC) will have the 3 confidential meeting rooms for mental health that will be fully operational in the reception area at WCC on July 24, 2023. They are doing the final work to include keys, furniture, and security walk through. |
| Develop guidelines for placement and care of individuals in need of the Close Observation Unit due to suicidality, meaning they have been identified as at risk for a suicide attempt. | As of July 2023, the workgroup is in the process of finalizing the recommended guidelines. Many of which have already been incorporated into Suicide Risk Assessment and Treatment Protocol for Mental Health Staff. |
| Develop report to allow for comparison of intake paperwork with mental health screenings to ensure all screenings are completed per policy with a process for regular reviews and establishment of a team to address any deficits. | This work is expected to be completed in October 2023. |
| DOC should urge county jurisdictions to complete and forward a transfer sheet with incarcerated individuals when transferred to state prison that would be reviewed by the intake nurse at each reception center. | A form was completed and provided to these jurisdictions with a request to use it. This has been challenging as there is no overarching agency that can compel counties to use this document. |
Challenges Unique to Prisons
It is also important to note that suicide is a complex and challenging health crisis that can be made more difficult to manage while operating in a prison setting. There are specific times of elevated risk associated with incarceration, such as admission to DOC, especially if the person is admitted directly to restrictive housing (solitary confinement). For these reasons, these are specific points in a person’s time of incarceration that mental health staff meet with them within a day of these events and complete a screening of mental health experiences, needs and potential suicide risk.
The means of self-harm and suicide are different in prison, and efforts are taken to identify and limit any means by which individuals in crisis may harm themselves. If there is a concern about a specific person being at high risk for suicidal behavior, they are then placed in a setting where they can be more closely monitored, be provided additional mental health support, and have restricted access to means to harm themselves.
Common Myths about Suicide
When considering how best to help someone experiencing a mental health crisis in prison, it is important to consider common myths about suicide, which apply both in communities and in prison.
The Mayo Clinic has published eight common myths about suicide, a few of which we will share here, however to read all eight visit its website.
Myth 1: Talking about suicide increases the chance a person will act on it.
Fact: Talking about suicide may reduce, rather than increase, suicidal ideation. It improves mental health-related outcomes and the likelihood that the person would seek treatment. Opening this conversation helps people find an alternative view of their existing circumstances. If someone is in crisis or depressed, asking if he or she is thinking about suicide can help, so don't hesitate to start the conversation.
Myth 2: People who talk about suicide are just seeking attention.
Fact: People who die from suicide have often told someone about not wanting to live anymore or they do not see the future. It's always important to take seriously anybody who talks about feeling suicidal. It's important to be kind and sensitive, and ask direct questions such as: "Are you thinking about hurting yourself?" "Are you thinking about suicide?" or "Do you have access to weapons or things that can be used as weapons to harm yourself?”
Myth 3: Suicide can't be prevented.
Fact: Suicide is preventable but unpredictable. Most people who contemplate suicide, often experience intense emotional pain, hopelessness and have a negative view of life or their futures. Suicide is a product of genes, mental health illnesses and environmental risk factors. Interventions targeted to treat psychiatric and substance use illnesses could save lives.
DOC’s Commitments to Suicide Prevention Moving Forward
Losing even one individual to suicide is one too many. Whether it is structural changes, policy changes, mental health screening improvements or training initiatives, DOC has undertaken a number of projects to even further improve mental health access for individuals and support in times of crisis. Suicide isn’t just a threat to the incarcerated. Corrections officers are also at much greater risk and have a higher occupational suicide rate. Improving conditions within our prisons, is essential for both those in our care and custody and those incarcerated in our prisons. Staff Psychologists and Critical Incident Stress Management Review teams are available for staff in need.
Many of DOC’s current initiatives to improve the experience for those incarcerated in prisons are opportunities to continue preventing suicide. Programs like Amend that improve communication between incarcerated individuals and staff, and the initiative to reduce restrictive housing by 90% in the next five years are big steps to improve overall mental health for those incarcerated within Washington state prisons.
The goal is to destigmatize mental health challenges, raise awareness for the support that individuals can gain access too and continue providing education and training to staff to best prepare them to support individuals experiencing a mental health crisis.
Whether it is a staff member who intervenes early on by noticing cues from an individual in crisis in order to get them help quickly or a staff member who is able to perform life saving measures after an attempt, DOC is committed to early intervention and mental health support for all individuals who need it.
Resources
Department of Corrections
- Amend: How We Create Better Neighbors
- PRESS RELEASE: DOC Pledges to Drastically Reduce Use of Solitary Confinement and Announces Closure of Minimum-Security Prison
- Suicide Prevention Posters (pdf) (500-PS003)
- Unexpected Fatalities
